Paula Tusiani-Eng is Executive Director of Emotions Matter, Inc., a non-profit organization dedicated to empowering individuals impacted by borderline personality disorder, and the co-author of “Remnants of a Life on Paper: A Mother and Daughter’s Struggle with Borderline Personality Disorder.”
May 18, 2018 - When doctors told my sister Pamela she might have borderline personality disorder (BPD) in 1998 at the age of 19, she wrote in her diary, “I wish I knew what was wrong with me. The doctor doesn’t even seem to know much about my diagnosis, which scares me. I am sick and need to be helped and treated correctly.”
In 1980, when BPD became an official mental health diagnosis in the Diagnostic and Statistical Manual of Mental Disorders-III, nine criteria were identified, including a pattern of unstable relationships, an unstable self-image, impulsivity, fears of abandonment, and self-harm.
Current research shows that BPD is a mental disorder caused by neurological impairment in the part of the brain that regulates emotions, thoughts and impulses. But many clinical professionals still lack sufficient education and training to properly treat it.
“Is it a real diagnosis, or just a character flaw?” some say, failing to legitimize personality disorders which don’t respond to traditional therapies or medications. Others dismiss BPD patients as “difficult or overly dramatic,” leading to misdiagnosis. Up to 70 percent of those diagnosed with BPD attempt suicide, and 10 percent die by suicide.
Pamela instinctively knew she needed better care. But the resources for treating BPD were scant in the late 1990’s. There weren’t enough long-term facilities, or doctors trained in BPD therapies. Sadly, Pamela lost her life in 2001 due to a rare adverse food and drug interaction involving a MAOI inhibitor that was being used to treat her depression. The medical professionals responsible for her life mismanaged her care because they did not understand best practices for personality disorders.
Thankfully, 17 years later, things have improved. New evidence-based treatments for BPD exist, such as dialectical behavior therapy, mentalization, transference-focused therapy, and general psychiatric management. Family treatments and educational workshops are now available.
But what good is effective treatment when most of the population can’t get it? Discrimination against BPD unfortunately still exists in society.
Individuals with BPD are routinely denied treatment coverage by health insurance companies.
Individuals with BPD are routinely turned away by clinicians who won’t treat them.
Individuals with BPD are routinely penalized at work, in court, or social service agencies who fail to recognize their serious mental illness as a disability which impairs their functioning.
BPD remains on the outside of federal mental health policy and funding. Innocent victims, like my sister and so many others are still suffering – and dying from it.
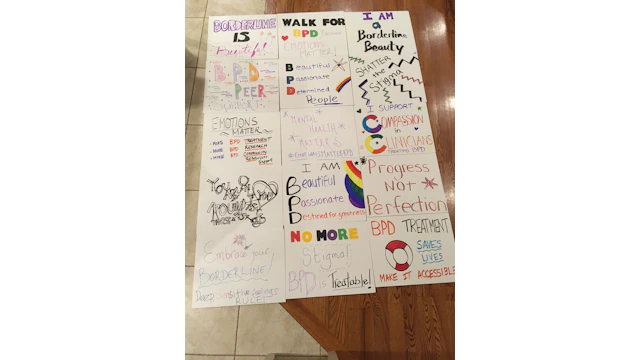
Emotions Matter, Inc., a 501c3 organization dedicated to BPD advocacy, is hosting the first ever Walk for Borderline Personality Disorder on Sunday, May 20, 2018, at Hudson River Park, Pier 40 in New York City. A grassroots group of individuals, families and clinicians will be walking along the border of New York and New Jersey, to help spread awareness of BPD, and encourage its acceptance as a mental health priority.
Speakers with lived BPD experience will be featured at the walk, including Stacy Pershall, author of “Loud in the House of Myself;” Syanne Centeno, former Miss Maryland; Carissa Wright, BPD Advocate from Western Australia; and members of the Emotions Matter Peer Leadership team.
If my sister was alive today, I would respond to her diary entry the way I respond to individuals with BPD who reach out to Emotions Matter:
“Pamela, you don’t have to be afraid about what is going on in your brain. I know it’s scary and feels awful right now, but we know what borderline personality disorder is, and there are trained clinicians who can help you. Treatment and community support exist, and you can access it. You can get better.”
Until I can say those words with integrity, knowing that every individual suffering from BPD can actually get the mental health care and community support they need, our work in spreading awareness of BPD must continue. I hope you’ll join us.