Each year, February is recognized as Black History Month. This year’s theme is “A Century of Black History Commemorations,” as we are celebrating the 100th anniversary of the observance, focusing on its impact on identity, pride, and equality, and encouraging exploration of Black life and history's role in transforming the modern world. It is a time of reflection.
As I reflect on my 30-plus years in the mental health field, I have seen changes and growth, particularly in our approach to suicide. We have made advancements in our understanding of the science of suicide prevention, such as developing better screening tools, exploring biological markers, and introducing mobile apps that encourage people to manage their mental health. We have invested heavily in suicide prevention research. And we have made strides in understanding the impact of suicide on society. But despite all our advancements, stigma remains a recurring theme. Shame, guilt, and reluctance to seek help often accompany mental health challenges. Stigma can manifest as negative attitudes toward others, but it can also be internalized in the form of negative beliefs or perceptions we may hold about ourselves. It can also be structural in the form of discriminatory policies that create systemic exclusion from opportunities like jobs, housing, or health care, thereby turning societal prejudice into concrete, harmful actions affecting individuals living with mental health challenges. Whatever form it takes, stigma can cause emotional and psychological distress, social withdrawal, and economic disadvantages that may increase challenges in a person’s life, or limit their ability to get help.
Because we recognize the negative impact of stigma on mental health, we often want to tackle it head on. We call it out, we prioritize it, and we vow to eliminate it. But I fear that we often fail to consider the root causes of stigma. Stigma is essentially a narrative, albeit a negative, misinformed, and often hurtful narrative. It is a narrative that is shaped, shared, and carried forward by a community. Stigma can originate as an explicit attempt to breed division and separation and to establish hierarchy; but stigma can also arise out of fear, ignorance, or collective trauma. In order to launch more targeted suicide prevention initiatives for everyone, we need to have a deeper understanding of the origins of stigma, including why it exists, how it developed, and why it may look different in historically marginalized communities.

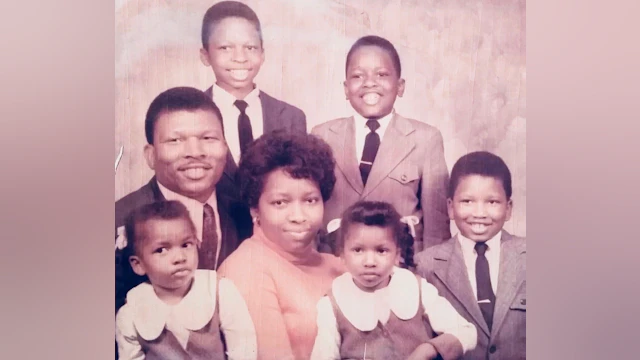
When I reflect upon my upbringing and the narrative given to me by my community, stigma clearly impacted my views. Growing up as a Black man in rural North Carolina, I was socialized to believe that Black people do not die by suicide; that it was not a problem for the Black community. My narrative was that in my community, “We are strong, we are resilient, and we survived slavery: therefore, we can survive anything.” I was also warned that Black men are often devalued when viewed as flawed mentally, physically, spiritually, or emotionally. This narrative encouraged me to avoid any association with mental health or mental health challenges.
In addition, being raised in a religious family, the son of a pastor, I was taught that people of faith don’t need therapy. It was an entrenched belief that experiencing anxiety or depression is a sign of spiritual weakness, and that the remedy is more prayer, or taking a “closer walk” with God. After all, our Sunday morning hymn was “Jesus on the Mainline,” not “therapist on the hotline.”
My rural community upbringing also influenced my narrative. From an early age, I learned the value of hard work and perseverance. I was taught that when you are down, you pull yourself up “by your bootstraps.” I was not afforded a “mental health day” when I was expected to show up at 6 a.m. for my summer employment on my uncle’s farm. And rather than today’s mantra of, “It’s okay to talk,” I often heard, “What happens in this house stays in this house.”

Stigma became normalized, in part because it was a convenient narrative, but also because the narrative was consistent and filled a void. In my community with a population today of just over 3,000 people, there were no psychiatrists. In my youth, I never met a psychologist or a social worker, but we did have plenty of churches. In hindsight, it made sense that we built a narrative based upon what was available to us. We built a narrative that projected strength in the face of adversity. The narrative handed to me was not intended to do me harm; it was intended to be empowering. It was intended to lift me out of despair. And keep in mind that the narrative that manifested into stigma went unchecked by research, literature, or the “experts in the field.” There was no narrative outside my community that challenged my misinformation. There were no advocacy organizations or campaigns in my community raising awareness about mental health and suicide. Stigma was given room to breathe.
Stigma campaigns, slogans, and catchphrases can be effective. I use them myself, but it is imperative we realize that when it comes to communities, it is difficult to change perception without acknowledging the origin of that perception. It is also difficult to erase stigma without addressing the fear that gave life to it and acknowledging the silence that gave it room to breathe.
We must be open to talking about mental health and suicide, recognizing that mental health challenges are nothing to be ashamed of, acknowledging that life is hard, and that we all need each other. For it is together that we eradicate stigma — in every aspect of our lives.